Cardiac Resynchronisation Therapy (CRT)
Background
Heart failure is the clinical syndrome that occurs when the heart is unable to pump enough blood to meet the body’s energy requirements. Symptoms include shortness of breath, dry cough, swelling in the ankles or legs, weight gain, fatigue, or palpitations.
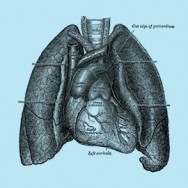
In a normal heart the ventricles (the lower two chambers) contract in a co-ordinated fashion to pump blood to the body and lungs. However in a patient with heart failure, often the left and right ventricles are out of sync and do not contract in a co-ordinated fashion. This is especially prevalent in patients with a type of conduction problem called left bundle branch block. When this occurs the left ventricle cannot pump the blood as effectively and it worsens the heart failure.
Cardiac resynchronisation therapy (CRT), also called “biventricular pacing”, is a special type of pacemaker that is used in heart failure to make the left and right ventricles contract in a more co-ordinated fashion. CRT has been shown to improve the symptoms of heart failure, the ability to exercise, the patient’s quality of life, and to reduce the number of hospitalisations.
The CRT device works in a similar way to pacemakers. It has two main components:
- A pulse generator, which generates electric impulses. It is made of a small computer and long-lasting battery.
- The leads, which transmit the electric pulses to the heart muscle. There are 3 leads that go to the right atrium (upper chamber of the heart), right ventricle, and via the coronary sinus to the left ventricle.
Patients with heart failure are also often at risk for abnormally fast, irregular heart rhythms. These rhythms can be life-threatening if not treated immediately. So most CRT devices are also able to function as Implantable Cardioverter-Defibrillators (ICD). This allows them to monitor and record the rhythm, slow down fast rhythms, and if necessary “shock” dangerous rhythms.
https://www.youtube.com/watch?v=7hEw4o06Fwc
About the surgery
In most cases CRT devices are inserted under general anaesthesia. A CRT device is about the size of a stopwatch. The most common site for implanting them is on the left side either above or below the pectoral muscle below the collar-bone.
Once the site has been prepared for the CRT device, the leads are then moved into position in the heart through the veins. This is done using image intensification (a special type of x-ray) to help the surgeon guide the leads into the correct position and the leads secured with an internal helix. Only the tips of the leads stay in contact with the heart. The ICD is then tested and the small incision where the ICD was inserted is sutured closed with dissolving stitches.
Recovery period
Patients usually stay overnight in hospital to ensure the ICD is functioning well and the patient’s heart rhythm is normal. There may be some mild pain, swelling, or tenderness in the area where the CRT device was placed, that can be relieved with over-the-counter medication. Patients normally return to their normal activates a few days after the surgery. However patients are advised to avoid vigorous activities or heavy lifting for about a month, and avoid driving for up to 6 months.
Risks of the surgery
CRT implantation is generally very safe. There is a small risk of bleeding, infection, damage to nerves, veins or lung, or the leads causing damage to the heart. Your surgeon will discuss the aims and risks of your procedure in more detail with you.
Monitoring
If the patient has a combination CRT-ICD device and they feel a shock they should contact their doctor within 24 hours or go to an emergency department right away.
CRT devices require checking on a regular basis, usually every 6 – 12 months to ensure problems are detected early and there is enough battery left. Checking is done from outside the body using a radiowave programmer, so no invasive procedures are required.


