Transcatheter Aortic Valve Implantation
Background
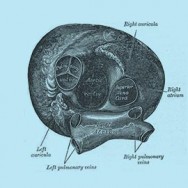
The aortic valve controls blood flow between the left ventricle and the aorta, the vessel that delivers oxygen-rich blood to the body. There are two main problems that can occur with the aortic valve: it can become hardened and narrowed (stenosis), or it can leak (regurgitation). The most common problem in the elderly is called age-related calcific degeneration, where the gradual buildup of calcium causes the valve to narrow. Symptoms of aortic stenosis include lightheadedness, chest pain, shortness of breath and fatigue. In patients who are at high-risk of complications in surgery, the aortic valve can be replaced by transcatheter aortic valve implantation (TAVI).
About the surgery
At Sydney Heart & Lung Surgeons we perform TAVIs as part of a “Heart Team”, which means that cardiothoracic surgeons, cardiologists, anesthetists, geriatricians, and nursing staff that are all involved in the patient’s care. The procedure is performed in a “hybrid theatre” with advanced imaging technology.
In TAVI, a biological (tissue) valve is mounted inside a stent (a circular wire mesh). The stent is then compressed so that it can fit inside a small delivery sheath (tube). The TAVI valve is then delivered to the aortic valve, the stent is expanded, and the biological valve inside begins to work. In TAVI the calcified leaflets of the patient’s diseased aortic valve are not removed, instead they are pushed to the side when the stent expands and help to lock the stent in place.
There are multiple ways of delivering the TAVI valve to the aortic valve position including:
- Transfemoral – The delivery sheath is inserted into the femoral artery in the patient’s groin, and the TAVI valve travels upwards through the artery to the aortic valve.
- Transapical – A 5-10cm horizontal incision is made on the left side of the chest below the nipple line, which provides direct access to the heart. The delivery sheath is then inserted in the apex of the heart and the TAVI valve inserted.
- Transaortic – A small incision at the top of the sternum (breast bone) is made and that the delivery sheath is inserted into the aorta (the large blood vessel that the aortic valve is in).
The “Heart Team” will assess each patient and decide what is the best approach to use. The transfemoral approach is the preferred because it is minimally invasive, however it is sometimes not possible because of peripheral vascular disease. A transapical or transaortic approach is then considered.
Recovery period
Patients usually stay in the intensive care unit for 1 – 2 days for monitoring, and then in the nursing unit for 6 – 7 days. Full recovery usually takes about ?2 months. Your surgeon will provide specific guidelines for your recovery and return to activities.
Risks of the surgery
TAVI is generally reserved for patients that are considered too high-risk for surgical aortic valve replacement. This is because it has been shown to be better than medical therapy, and the risk of death is lower than surgery in high-risk patients. However the risk of stroke is slightly higher in TAVI.
There are a number of other specific risks, including a leak around the TAVI valve (paravalvular regurgitation), damage to the heart around the valve (aortic root injury), kidney injury, arrhythmias and pacemaker implantation, bleeding and possibly death. As with all invasive procedures there are also some general risks, including wound infection, and reactions to the anaesthetic.
For more information please visit:
Cleveland Clinic Percutaneous Valve Interventions
All patients should consult their cardiothoracic surgeon for specific information about their medical condition and surgery.

